The human brain is wired with natural checks and balances that control negative emotions, but breakdowns in this regulatory system appear to heighten risk of violent behavior, according to findings of a study by UW–Madison psychologist Richard Davidson.
As part of a special report on violence in the July 28 issue of the journal Science, Davidson and colleagues analyzed brain imaging data from a large, diverse group of studies on violent subjects and those predisposed to violence. The studies focused on people diagnosed with aggressive personality disorder, those with childhood brain injuries and convicted murderers.
Researchers found common neurological threads among these more than 500 subjects in the brain’s inability to properly regulate emotion. The study focused on several interconnected regions in the prefrontal cortex of the brain, areas defined in Davidson’s previous work as an essential control mechanism for negative emotions.
A similar brain process has been implicated in a number of mental health problems, including depression and anxiety disorders. Davidson says this newfound connection between violence and brain dysfunction opens a new avenue for studying and possibly treating violence and aggression.
“We are placing the question of violence right in the middle of our basic research on the neurobiology of emotion, because our previous insights in this area give us tremendous leverage to understand the root causes of violence,” Davidson says. “There never has been a theoretical framework to make sense of this before.”
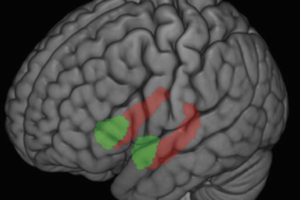
One of the core findings, Davidson says, deals with the interplay between several distinct brain regions, namely the orbital frontal cortex, the anterior cingulate cortex and the amygdala. The orbital frontal cortex plays a crucial role in constraining impulsive outbursts, while the anterior cingulate cortex recruits other brain regions in the response to conflict. The amygdala, a tiny but highly influential portion of the brain, is involved in the production of a fear response and other negative emotions.
Davidson and colleagues Katherine Putnam and Christine Larson found that normal brain activity in the orbital and anterior regions were blunted or entirely absent in many of the study groups, while the amygdala showed normal or heightened activity. The inability of the two brain regions to effectively counteract the response of the amygdala may help explain how threatening situations can become explosive in some people.
“We are placing the question of violence right in the middle of our basic research on the neurobiology of emotion, because our previous insights in this area give us tremendous leverage to understand the root causes of violence. There never has been a theoretical framework to make sense of this before.”
A major strength of the research is in the range of people studied and the consistency of the results, Davidson says. The researchers found dysfunction in common brain regions in reviews of brain imaging data from 41 murderers, from a study group suffering from aggressive impulsive personality disorder, and from a group diagnosed with antisocial personality disorder.
They also reviewed data from two individuals who suffered early damage to the two regions of the brain in question. Those individuals, injured early in life, both showed histories of verbal and physical abusiveness and intermittent, explosive bursts of anger.
The research paper also described a large group of subjects who have a genetic deficit that causes a disruption in the brain’s serotonin levels. The serotonin system employs many of the brain regions described earlier and a disruption of the system has been linked to increased aggression. Davidson’s analysis showed that these emotion-controlling brain regions showed less activity in the individuals who carried this genetic abnormality.
Davidson stresses that the research points to both genetics and poor environmental history as potential contributors to impulsive violence, and together they present a “double whammy” that put people at much greater risk. “These parts of the brain are particularly responsive to experiential shaping,” Davidson says.
The study may recast the way society looks at impulsive violence, by defining it as a mental health issue. “Emotion regulation is extremely significant for a whole constellation of problems people encounter,” he says.
The long-term implications of the study will be in the realm of new treatments, Davidson predicts, that will combine targeted behavioral interventions with drug therapies, in much the same way depression and anxiety disorders are treated.
“Given what we know about brain plasticity and the fact that the brain really can change in response to experience, we have good reason to expect that these treatments may, in fact, have beneficial consequences,” Davidson says.
While the research points to emotion regulation deficits as a “smoking gun” in impulsive violence, Davidson cautions that science is a long way from developing any preventive strategy for at-risk populations. Davidson’s future studies will explore this complex brain process in much greater detail, through the use of imaging technologies such as magnetic resonance imaging (MRI) and positron emission topography (PET) used in tandem for high-resolution, real time images of brain function.
Davidson is director of the Wisconsin Center for Affective Science and directs the W.M. Keck Center for Functional Brian Imaging. His research is supported by the National Institute of Mental Health.
– Brian Mattmiller