The University of Wisconsin–Madison has received a $2.5 million four-year grant from the National Institutes of Health (NIH) to establish a research network on the plasticity of well-being and to develop innovative measures of the key pillars of well-being. The network, funded by the National Center for Complementary and Integrative Health, is one of five research networks across the country that NIH is supporting to advance our understanding of emotional well-being.
Faculty and experts from the Center for Healthy Minds are leading the effort, which will include pilot research projects, collaborations, and scientific meetings focused on interventions and prevention strategies with partners at UW–Madison, Northwestern University and Massachusetts Institute of Technology (MIT). The goal of the network is to identify ways to measure people’s emotional health and well-being in everyday life and understand how flexible those aspects of well-being could be with effective, culturally relevant interventions and training.
Emotional well-being is, at its core, living a good and meaningful life. One purpose of these networks is to better define emotional well-being and to connect the definition to established research.
Collaborators of the UW–Madison network bring expertise in a broad range of fields, including psychology, neuroscience, microbiology, community-based research, electrical and computer engineering, population health and biology, and the humanities.

“Well-being has been treated as a static variable in science. This network is predicated on the idea that the way we’ve been doing things isn’t the whole story and that well-being is plastic and something we can modify,” says Richard Davidson, principal investigator of the grant, director of the Center for Healthy Minds, and the William James and Vilas Professor of Psychology and Psychiatry at the University of Wisconsin–Madison. “We’ll be focusing on the core pillars of well-being that exhibit plasticity – What are they, and how can we measure them in ways that are robust and go beyond self report measures? By the end of the four years, we hope to find out and find what strategies work, and to ensure the measures and interventions are applicable to all people and not a specific subgroup.”
"By the end of the four years, we hope to find out and find what strategies work, and to ensure the measures and interventions are applicable to all people and not a specific subgroup.."
Conducting more comprehensive mobile health studies where people can take part at home instead of coming into the lab could not only increase the diversity and number of people in studies, but it could also strengthen the scientific results, especially in the current environment where telehealth and mobile interventions are being accelerated by and will likely outlast the pandemic. This is especially true when it comes to gathering samples and data on health and well-being that normally require a visit to the lab, but are now being developed to complete at home.
There are new avenues to understanding well-being that could be explored. For instance, are there clues in blood samples or gut bacteria that correlate with a person’s emotional well-being or with changes from before to after an intervention? How might more passive data collection through wearable technology paint a broader picture about someone’s mental and physical health?

These are some of the questions and exciting angles the network can explore, says Heather Abercrombie, scientific director at the Center for Healthy Minds, who is the scientific coordinator of the network. She says there’s plenty to learn about when it comes to moving one’s skills towards greater emotional well-being and how those skills can be shaped for the better.
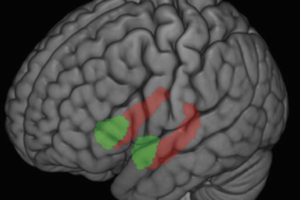
“We really need to find a way to measure how skills related to emotional well-being move toward capacities and then competencies, like how we gradually learn a new language or how to ride a bike with practice” she says. “This gets at what we call plasticity – our brains’ and bodies’ ability to change.”
Abercrombie says the shift toward personalized medicine – medical treatment tailored to a specific person – has yet to be explored for emotional well-being and mental health. In addition, exploring how culturally enriched interventions based on a person’s race, cultural and lived experiences can ensure that the research outcomes and tools from the network are equitable and relevant across communities.
"We really need to find a way to measure how skills related to emotional well-being move toward capacities and then competencies, like how we gradually learn a new language or how to ride a bike with practice."
Expert Partners
Below are expert partners in the network and their approaches to this work:
UW–Madison Team
Heather Abercrombie, Scientific Director at the Center for Healthy Minds

Expertise: Psychology, psychiatry, neuroscience, well-being interventions
Tony Chambers, Director of Equity, Inclusion and Innovation at the Center for Healthy Minds

Expertise: Community-based research, education, mental health equity and inclusion
Richard Davidson, Founder and Director of the Center for Healthy Minds, William James and Vilas Professor of Psychology and Psychiatry

Expertise: Psychology, psychiatry, neuroscience, well-being interventions
John Dunne, Distinguished Chair in Contemplative Humanities at the Center for Healthy Minds and Professor of Asian Languages and Cultures

Expertise: Contemplative science, well-being interventions, Religious Studies, Philosophy
Simon Goldberg, Assistant Professor of Counseling Psychology and faculty at the Center for Healthy Minds

“For more than a decade, we have seen evidence suggesting that meditation training can improve mental health. The bottleneck has been limited access. While there is much yet to be learned,” there’s a “growing body of research suggesting mobile apps are a viable way to meaningfully increase access to these strategies.”
Expertise: Mindfulness-based interventions, psychology, psychiatry, mobile health applications
Jo Handelsman, Director of the Wisconsin Institute for Discovery, Vilas Research Professor, and Howard Hughes Medical Institute Professor in the Department of Plant Pathology

Expertise: Molecular biology, the microbiome
Robert Nowak, Professor of Electrical and Computer Engineering

Expertise: Machine learning, data optimization
Melissa Rosenkranz, Distinguished Chair of Contemplative Neuroscience, Center for Healthy Minds, Assistant Professor of Psychiatry

Expertise: Psychology, neuroscience, contemplative science, well-being interventions, brain-immune interactions
Earlise Ward, Professor of Nursing, Faculty Director UW Carbone Cancer Center Health Disparities Initiative, and Faculty Director of the Morgridge Center for Public Service

Expertise: Community-based clinical research, mental health interventions, mental health promotion among African American adults
Northwestern University Team
Thomas McDade, Carlos Montezuma Professor of Anthropology and Faculty Fellow, Institute for Policy Research

Expertise: Stress; health inequities; developmental origins of health and disease; “field-friendly” biomarker methods
Greg Miller, Louis W. Menk Professor; Institute for Policy Research and Department of Psychology

Expertise: Health inequities; childhood origins of disease; life stress; immune function; resilience
Massachusetts Institute of Technology Team
Rosalind Picard, Professor of Media Arts and Sciences, Director and Founder of Affective Computing Research Group, MIT Media Lab, Faculty Chair of Mind+Hand+Heart Initiative

Expertise: Affective and wearable computing, machine learning and artificial intelligence, digital health, human-computer interaction
“I’m thrilled to partner with this all-star team and collaborate on new ways to advance well-being. Sometimes, technology has been developed that injures well-being; in contrast, this network will use technology to help people improve well-being.”
–Marianne Spoon